Task force meets and starts discussion on solving EMS challenges in Orleans
ALBION – A task force of about 30 local officials, fire department representatives and ambulance service providers met for the first time last week to discuss challenges to the local EMS system which often faces drop calls, slower response times, financial challenges and a shortage of manpower.
“We’re coming into this with an open mind,” Justin Niederhofer, the EMS coordinator for the county, told about 30 local officials, fire department representatives and ambulance providers during a meeting last week at the Orleans County legislative chambers. “We don’t know what the solution is.”

Orleans County Legislator Skip Draper, head of the county’s Public Safety Committee, convened the task force and urged the group to push for solutions.
He urged the group to put the past behind them, especially with dropped calls, and forge solutions for the future. A dropped call is a request for service but the agency can’t get there and the call is sent to another responding agency.
The task force members will need to decide what is an acceptable response time for an ambulance in their community, and work towards that goal. Niederhofer said it is “unrealistic to think 100 percent of the calls 100 percent of time.”
There are four ambulance providers serving the county – Medina Fire Department, COVA, Monroe Ambulance and the Kendall Fire Department – and all operate differently.
All four have seen their response times increase from 2018 to 2021.
- COVA’s average response increased from 6:52 for 2,010 calls in 2018 to 8:10 for 2,214 calls in 2021. Dropped calls increased from 53 to 125 during that time period.
- Kendall averaged a 9:19 response for 113 calls in 2018. That was up to 10:47 for 201 calls last year. Dropped calls up from 16 to 71 during those years.
- Medina had a 6:34 average response time for 2,333 EMS calls in 2018, which increased to 7:22 for 2,311 calls in 2021. Dropped calls up from 7 in 2018 to 21 last year.
- Monroe Ambulance had a 12:13 average response time for 726 calls in Orleans County in 2018. That was up to 16:09 for 950 calls in 2021. Monroe’s drop calls in Orleans increased from 19 in 2018 to 79 in 2021.
Medina Fire Department serves the west end of the county – Shelby, Ridgeway, Medina, Lyndonville and Yates – and provides the service with the only paid career fire department in the county.

Dale Banker, the county’s emergency management coordinator, said more calls are going to mutual aid, which further strains the system and often results in a slower response.
The department has 21 paid firefighters who respond to fire and EMS calls. Fire Chief Matt Jackson said the department loses valued members to suburban departments that pay about $20,000 more annually.
Medina took over as the primary ambulance provider in 2007 for the western end of Orleans County. Rural Metro had the contract before that.
Medina responded to 2,616 total calls in 2021 with two-thirds of those EMS calls. Medina FD is increasingly being asked to provide mutual aid outside its primary service area, going into central Orleans, eastern Niagara and even Genesee County as many areas have manpower shortages.
Jackson said Medina will only take those calls if it has another available crew to respond to an emergency in Medina and western Orleans.
The Kendall Fire Department is the last volunteer fire department running an ambulance in Orleans County. Clarendon, Holley, Carlton, Albion and Shelby have all disbanded their ambulances.
Kendall has seven emergency medical technicians right now, with another in training, said Shelby Willis, EMS captain for the Kendall Fire Department.
“We have every intention of keeping up with our ambulance but staffing is the main problem right now,” Willis said.

Shelby Willis, EMS captain for the Kendall Fire Department, said the volunteer group isn’t able to bill for its services and relies on fundraisers.
The training requirements to be an EMT and paramedic have gone up, and ambulances have to drive farther, often into Rochester and Buffalo and then wait longer for hospitals to accept the patients. The whole process makes it much more demanding of time from the volunteer staff.
“We’re volunteers and we can’t make every call,” Willis said. “The transports are farther. Sometimes it takes 2 to 3 hours. We’re giving up a lot of time.”
Kendall is talking with the Murray Fire District about crew sharing, with the possibility of having an ambulance stationed in Murray with Murray firefighters helping to staff it.
Kendall, because it is a volunteer ambulance, can’t bill for its services. It relies on donations and fundraisers.
Monroe Ambulance responds to about 35,000 calls in Monroe County, eastern Orleans and Wyoming County.

John Williams is Deputy Chief at Monroe Ambulance. Hospitals are pulling many paramedics away with higher pay and an easier workload, he said.
The company is down 37 percent of its paramedics in the past two years. Many have left Monroe to work in hospitals where they are paid $35 an hour to do blood draws, said John Williams, deputy chief at Monroe Ambulance.
Monroe has launched an in-house EMT academy and has stepped up recruiting efforts at local high schools. It also is taking with Monroe Community College about a program to train paramedics.
Monroe Ambulance also is offering signing bonuses and boosting pay. Right now the average wage is $17.52 an hour for an EMT and about $25 for a paramedic.
Monroe has been hurt by people not paying their ambulance bills, and what is often a two-hour wait at hospitals to drop off a patient. That ties up the crew and leads to dropped calls for other emergencies, Williams said.
Monroe doesn’t keep an ambulance stationed in Orleans.
“The economics are not feasible for us to dedicate an ambulance to Orleans County,” he said.
Central Orleans Volunteer Ambulance is a non-profit organization based in Albion. The organization has struggled financially due to low Medicaid/Medicare reimbursement rates, patients who keep their insurance checks instead of directing them to COVA, and a lack of any tax support, said Wade Schwab, a paramedic and past president for COVA.
“It’s been a heckuva struggle,” Schwab said. “The biggest challenge is financial.”
Wade Schwab, a paramedic at COVA and past president, said the organization faces financial challenges. He advocates for assessing each household in central Orleans – Barre, Albion, Gaines and Carlton – $25 a year to keep COVA viable.
He said there is about $90,000 owed COVA in 2021 from unpaid bills. Turning unpaid bills into collections often “gets you nowhere.”
The longer wait times at hospitals also occupy an ambulance crew for more time, making them unavailable for other calls.
COVA has meet with local government leaders from the four central Orleans towns of Barre, Albion, Gaines and Carlton as well as the Village of Albion to dicuss an ambulance taxing district. None have moved to help COVA with the financial challenges, Schwab said.
COVA has suggested a $25 fee for each of the 7,793 households in central Orleans, which would raise $193,675.
With that funding, COVA could increase staff and put more ambulances in service, Schwab said.
Right now, state law limits an ambulance taxing district to a single town. COVA would like a multi-town taxing district for the four towns, or each town could perhaps create their own taxing district for an ambulance service. Schwab said COVA officials have met with state legislators to help with the issue, as well as to have insurance checks sent directly to COVA, but haven’t had much followup.
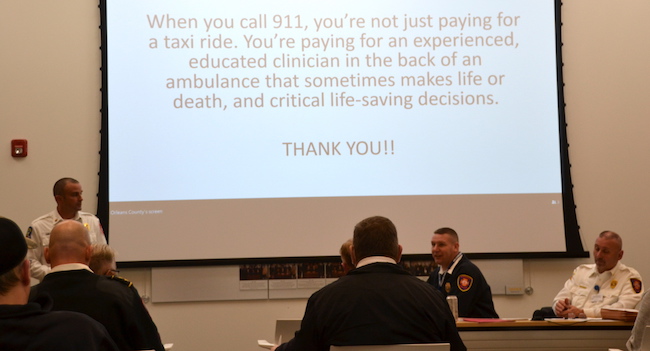
Schwab said the EMS staff should be paid more, given the training and responsibility. Right now, he said, Wegmans and Tim Hortons can offer similar pay for far less stress.
Some counties facing an EMS crisis have created county crews to supplement the local ambulance providers. Niederhofer and Dale Banker, the emergency management coordinator, said they would bring in officials from other counties who have tried that to hear how that has been working.
Schwab interjected that the county would be better served to assist its existing ambulance providers rather than create a new entity.
He said the county already has a great foundation for responding to EMS calls.
Justin Niederhofer, the county’s EMS coordinator and deputy emergency management coordinator, said the local EMS system has experienced more dropped calls and slower response times in the past year.
“We have hard-working professionals in the Medina Fire Department, Monroe Ambulance, COVA and Kendall, we just need a little help, Schwab said.
County Legislator Skip Draper convened the meeting as head of the County’s Public Safety Committee. He hears throughout the state that emergency services are collapsing.
The task force needs to offer solutions for the immediate problem and also look to future challenges. He said Medina FD is currently considered a model, but even that department is being in many directions and its future success is not a guarantee.
“Even though it’s working in some areas it’s still fragile,” Draper said about the EMS system.
The task force will next meet March 16 and will return with a survey about acceptable response times for different severities of emergency, whether advanced life support with paramedic level of care or basic life support at EMT level of care.
Jack Welch, the county chief administrative officer, said the local town and village leaders need to be part of solving the problem.
“We need buy-in from the municipalities,” Welch said. “What is acceptable service? We need to agree what the problem is.”