‘Person-first approach’ urged to mitigate effects of substance use stigma
By Mike Pettinella, GCASA Publicist
ALEXANDER – Attitudes toward substance use disorder and words that reflect those attitudes can have a tremendous effect on the recovery process of those struggling with addiction.
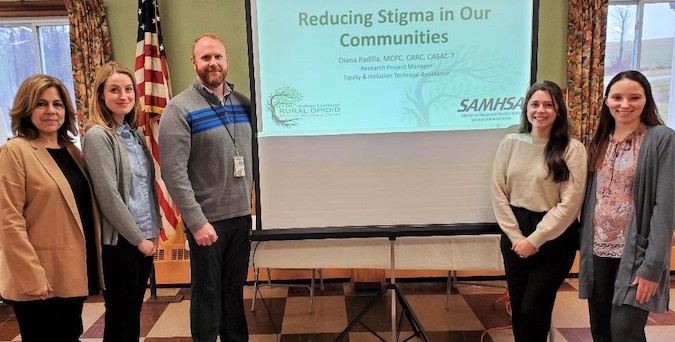
“Stigma is defined as a mark of disgrace and that (disgrace) is a pretty powerful word,” said Diana Padilla, a longtime behavioral health specialist who was in Genesee County on Wednesday to present a training seminar for social workers and providers at the Alexander Recreation & Banquet Facility.
Padilla, in her 90-minute “Reducing Stigma in Our Communities” presentation, provided tools for counselors to counteract the negative connotations associated with substance use and mental illness.
A research project manager at the New York State Psychiatric Institute, Division of Substance Use Disorders, Columbia University Medical Center, Padilla communicated that stigma against people with substance use disorders can create barriers to treatment, such as an increase in shame and isolation from family, friends and community, and treating those with addiction as criminals.
She bemoaned the fact that the healthcare and judicial systems have not fully recognized that substance use disorder is an illness, and that recovery is possible.
“Stigma can lead to more substance use disorder and people can lose hope,” she said. “It really becomes a vicious cycle.”
Padilla said she has seen how health insurance companies and the law continue to view substance use disorder as a “result of a moral weakness and flawed character.”
She noted that some providers blame the individual for causing the problem and will reject treatment coverage, which can lead to substandard, non-science-based care.
When it comes to mental health treatment, Padilla said statistics show that stigma prevents 40 percent of people with anxiety or depression from seeking medical help and affects people in treatment even when their mental health problem is a distant memory.
To combat stigma, she encouraged counselors to utilize “people-first language” in their interactions with their clients:
- Speak or write the person first, then the disability, i.e., Sam is a “person with a disability,” or “Sheila is visually impaired…”
- Emphasize abilities or accomplishments, not limitations.
- When communicating about a group, “individuals with disabilities.”
- Allow and expect that individuals with disabilities will speak for themselves.
- Be careful not to idealize people who have disabilities as being brave simply because they have a disability.
In recent years, there has been a shift toward supportive and affirming language used by public health professionals, she said.
“By using the term, substance use disorder (instead of substance abuse or addiction), it meets a diagnostic criterion,” she said.
Padilla promoted “trauma-informed care” as a key component to successfully reaching someone with substance use disorder and/or mental illness.
She referred to the Adverse Childhood Experience study that reveals a direct link between traumatic experiences at an early age to subsequent alcohol and drug problems. According to the ACE study, 64 percent of adults have faced one adverse childhood experience (emotional, physical or sexual abuse) and 40 percent have faced two or more adverse childhood experiences.
“A person with four or more ACEs is five times more likely to develop substance use disorder,” she pointed out.
It is important for counselors to understand the impact of traumatic events upon their clients’ lives, Padilla said, and to adhere to the guiding principles of trauma-informed care – safety, transparency, peer support, collaboration, empowerment and cultural, historical and gender issues.
“Empowerment, giving the client a voice and a choice, can make a huge difference,” she said. “We should support those choices even when we don’t totally agree.”
In closing, Padilla shared that people are more likely to get treatment and recover when their families, friends, providers, and communities support them without judging them.
“We can choose supportive, respectful, and nonjudgmental words that treat people with respect and compassion,” she said.
The training seminar was hosted by the GOW (Genesee Orleans Wyoming) Opioid Task Force and Genesee & Orleans County Health Departments and supported by the HEALing Communities initiative.