Gillibrand details impact on health insurance hikes for New Yorkers with ACA
In Orleans County individuals face $1,251 increase for year, while family of 4 would pay $2,547 more
Press Release, U.S. Senator Kirsten Gillibrand
WASHINGTON, D.C. – Today, U.S. Senator Kirsten Gillibrand (D-NY) held a virtual press conference to discuss the impact of rising health insurance premiums on New Yorkers across the state and to call on Republicans to extend the health insurance subsidies that help many Americans get care at a price they can afford.
Editor’s Note: In Orleans County, Gillibrand said single individual making $65,000 or less would see a 31.7 percent increase, from $329.46 to $433.76 a month, a $1,251.60 increase for the year.
For a family of four in Orleans County making $130,000 or less, the monthly cost goes up by 20.7 percent from $1,023.96 to $1,236.22 a month, a $2,547.12 increase for the year, according to data from Gillibrand.
“At least 1.6 million New Yorkers in every corner of our state are on the brink of seeing their premiums skyrocket – all because congressional Republicans refuse to extend the health care assistance that families rely on,” Gillibrand said. “This is a Republican-manufactured health care crisis that low- and middle-income New Yorkers simply cannot afford.”
Without an extension, Affordable Care Act enhanced tax credits will expire at the end of 2025, causing 20 million Americans to see a sudden increase in their health insurance costs. This includes at least 1.6 million New Yorkers, who will face an average yearly increase of $1,360 in the amount they pay for their premiums, with people in some counties experiencing far greater increases.
“Democrats stand ready to negotiate a bipartisan deal to keep health care costs low and reopen the government, but we need Republicans to come to the table,” Gillibrand said. “I’m calling on my Republican colleagues to prioritize American families over billionaires and end this crisis.”
Gillibrand emphasized the immense strain that this will put on working families and the dire need for Republicans to work with Democrats to address the looming health care crisis and end the government shutdown. Enrollees in New York State are already receiving notices of premium hikes ahead of the start of open enrollment on November 1st, underscoring the importance of extending the subsidies immediately.
Health insurance premiums are expected to increase by double- or triple-digit percentages in all of New York’s 62 counties if President Trump and congressional Republicans fail to extend ACA subsidies.
A county-by-county breakdown of the expected premium increases for the lowest-cost ACA plans can be found at gillibrand.senate.gov/trumphealthcareincrease.



























 Vaping or using e-cigarettes is a growing and urgent public health concern in Genesee and Orleans counties.
Vaping or using e-cigarettes is a growing and urgent public health concern in Genesee and Orleans counties.


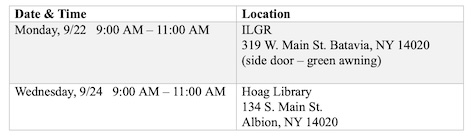 BATAVIA – The Independent Living of the Genesee Region, in partnership with the Genesee and Orleans County Health Departments, is pleased to announce an upcoming focus group dedicated to the families and caregivers of Children and Youth with Special Health Care Needs (CYSHCN).
BATAVIA – The Independent Living of the Genesee Region, in partnership with the Genesee and Orleans County Health Departments, is pleased to announce an upcoming focus group dedicated to the families and caregivers of Children and Youth with Special Health Care Needs (CYSHCN).


 As the summer days grow shorter and the crisp scent of autumn fills the air, families everywhere are preparing for another exciting school year. Whether you’re a student stepping back into the classroom, a teacher setting up for the months ahead, or a parent adjusting to a new routine, the start of the academic year brings both challenges and opportunities.
As the summer days grow shorter and the crisp scent of autumn fills the air, families everywhere are preparing for another exciting school year. Whether you’re a student stepping back into the classroom, a teacher setting up for the months ahead, or a parent adjusting to a new routine, the start of the academic year brings both challenges and opportunities.